Physiology of Gas Exchange
Overview of Hypercapnia
- Definition of Hypercapnia
- PaCO₂ is directly proportional to rate of CO₂ production (VCO₂)
- PaCO₂ is inversely proportional to rate of CO₂ elimination by lung -- alveolar ventilation
- Hypercapnia 2/2 increased CO₂ production (VCO₂)
- Increased metabolic rate
- Increased activity
- Sepsis
- Thyrotoxicosis
- Metabolizing of carbohydrates
- Increased metabolic rate
- Hypercapnia 2/2 decreased alveolar ventilation (\(V_A\))
- Decreased minute ventilation
- Increased VD/VT (i.e. physiologic dead space) with stable minute ventilation
- Rapid, shallow breathing
- Clinical Effects of Acute Hypercapnia
- Decreased level of consciouness
- PaCO₂ >60-70 mmHg in normal individuals
- PaCO₂ >90-100 mmHg in patients with chronic hypercapnia
- Increased cerebral blood flow, ICP
- Decreased myocardial contractility
- Decreased diaphragmatic function
- Shift oxyhemoglobin dissociation curve to the right
- Signs & Symptoms
- Decreased level of consciouness
Etiology of Hypercapnic Respiratory Failure
- Broken link in the chain of events
- Central respiratory center → spinal cord → motor neurons → neuromuscular junction → respiratory muscles → chest wall → lung
Central Respiratory Drive
- Decreased respiratory drive
- Sedative
- Opioid overdose
- Encephalitis
- Stroke
- Cheyne-Stokes Respiration
- Most common with heart failure, high altitude, and neurologic disease
- Biot Respiration
- Irregular clusters of breaths and apnea
- Lesion of upper pons or lower medulla
- Cheyne-Stokes Respiration
- Obesity hypoventilation syndrome
- Sleep apnea (central sleep apnea & obstructive sleep apnea)
- Congenital central alveolar hypoventilation
- Hypothyroidism
- Myxedema coma → depressed hypercapnic ventilatory drive & hypoxic ventilatory drive + respiratory muscle weakness & compromise of the upper airway
- Metabolic Alkalosis
Spinal Cord, Nerves, Neuromuscular Junction
- Disorders of Spinal Cord
- Direct Spinal Cord Injury
- Traumatic spinal cord injury -- 50% of motor vehicle accidents, neurologic progression over hours
- Cervical spinal cord injury & respiratory muscles
- Phrenic nerve to diaphragm: C3-C5
- Scalene muscles: C4-C8
- Sternocleidomastoid, trapezius: C1-C4; CN XI
- Complete injury above C3 = ventilatory failure
- Injury at C3, C4, C5 -- often wean from ventilator
- Amyotrophic Lateral Sclerosis
- Respiratory muscle weakness & progressive respiratory failure
- Combination of upper motor neuron and lower motor neuron disease
- upper motor neuron -- degeneration -> weakness, hyperreflexia, spasticity
- lower motor neuron -- degeneration -> weakness, atrophy, fasciculation
- Involvement of bulbar nerves -- Dysphagia, aspiration, laryngospasm
- Tetanus
- Caused by toxin-producing anaerobe Clostridium tetani
- Retrograde transport of exotoxin up axons to brainstem and spinal cord
- Blocks inhibitory neurotransmitters
- Results in: spastic paralysis especially laryngeal muscles and respiratory muscles
- Treatment: tetanus immune globulin, muscle relaxants, supportive (debridement, antibiotics, mechnical ventilation)
- Direct Spinal Cord Injury
- Disorders of Peripheral Nerves
- Guillian-Barre Syndrome
- Diphtheria
- Porphyria
- Tick paralysis
- Ciguatera fish poisoning
- Critical illness polyneuropathy
- Disorders of Neuromuscular Junction
- Myasthenia Gravis
- Eaton-Lambert Syndrome
- Organophosphate Poisoning
- Botulism
- Tick paralysis
- Snake venom -- including copperheads, moccasins, rattlesnakes
- Drugs: aminoglycosides, fluoroquinolones, anti-arrhythmics, phenytoin, lithium
- Hypermagnesemia
- Hypocalcemia
Respiratory Muscles & Chest Wall
- Respiratory Muscle Weakness
- Etiology
- Pre-existing
- Neuromuscular junction
- Malnutrition
- Hyperinflation
- Endocrine
- Hyperthyroidism
- Hypothyroidism
- New-onset
- Metabolic
- Hypokalemia
- Hypophosphatemia
- Acidosis
- ICU-Acquired Weakness
- Mechanical ventilation
- Metabolic
- Pre-existing
- Clinical features
- Decreased vital capacity
- Increased residual volume
- expiratory muscles → decreased expiratory reserve volume
- Decreased total lung capacity
- inspiratory muscles → decreased inspiratory capacity
- Further decrease in vital capacity when supine
- Decrease in maximum expiratory peak flow and maximum inspiratory peak flow
- Results in hypercapnia when strength is <40% predicted
- Desaturation, hypercapnia during REM sleep & in supine position
- Etiology
- Disorders of the Chest Wall
- Results in decreased chest wall compliance & reduced tidal volume (increased VD/VT)
- Hypercapnia exacerbated by
- reduced ventilatory drive
- muscle weakness
- Kyphoscoliosis
- Most patients with angle >90 degrees have hypercapnia
- Obesity Hypoventilation Syndrome
- Management of hypercapnic respiratory failure in morbid obese patients
- Identify and manage precipitating causes
- Non-invasive positive pressure ventilation
- improves ventilation → reduces work of breathing
- recruits atelectatic lung → improves V/Q matching → better oxygenation
- improves upper airway patency
- Head up (reverse Trendelenburg) position
- Management of hypercapnic respiratory failure in morbid obese patients
Lung
- Hypercapnic respiratory failure in patients with airflow obstruction
- Acute hypercapnic respiratory failure 2/2 COPD
- Advanced COPD patients have a difficult time overcoming new infections like pneumonia
- Fever causes increased VCO₂ and/or increased VD (due to pneumonia) → increased minute ventilation (by increasing RR) → decreasing expiratory time and increasing air trapping → increased work of breathing, fatigue → acute respiratory failure
- Goal: rest, relief of air trapping
- Non-invasive positive pressure ventilation
- Acute hypercapnic respiratory failure 2/2 status asthmaticus
- Development of dynamic hyperinflation
- Bronchospasm, airway inflammation, mucous plugging → airflow obstruction → prevents gas emptying
- New breath initiated before previous breath empties → increasing functional residual capacity
- Dynamic hyperinflation develops when the time needed to deflate the lung to normal FRC between breaths is insufficient
- i.e. auto-peep
- Effects of dynamic hyperinflation
- Moves diaphragm downward and at a mechanically disadvantageous position
- Incomplete alveolar gas emptying → elevated alveolar volume & alveolar pressure (intrinsic PEEP or auto-PEEP)
- Auto-PEEP represents a threshold pressure that must be overcome before inspiratory flow can occur → increasing work of breathing
- Ventilator adjustments for airflow obstruction
- Deliver adequate oxygenation
- Primary goal = increase expiratory time (i.e. time needed to exhale)
- Sedate patient to slow the respiratory rate
- Set lower RR -- most effective method
- Set lower tidal volume → less volume to exhale
- Increase inspiratory flow rate to deliver air more rapidly thus more time for exhalation
- Development of dynamic hyperinflation
Capnography
- Monitoring exhaled CO₂
- Phases in measurement of exhaled CO₂
- Phase 1: no exhaled CO₂ -- end inspiration to early exhalation of dead space gas from proceeding breath
- Phase 2: rise in exhaled CO₂ during the mixing of dead space gas and emptying of alveoli with transition to
- Phase 3: reflects the alveolar plateau as alveoli empty, reaching a maximum exhaled CO₂ immediately prior to
- Phase 4: the rapid fall in CO₂ during inspiration
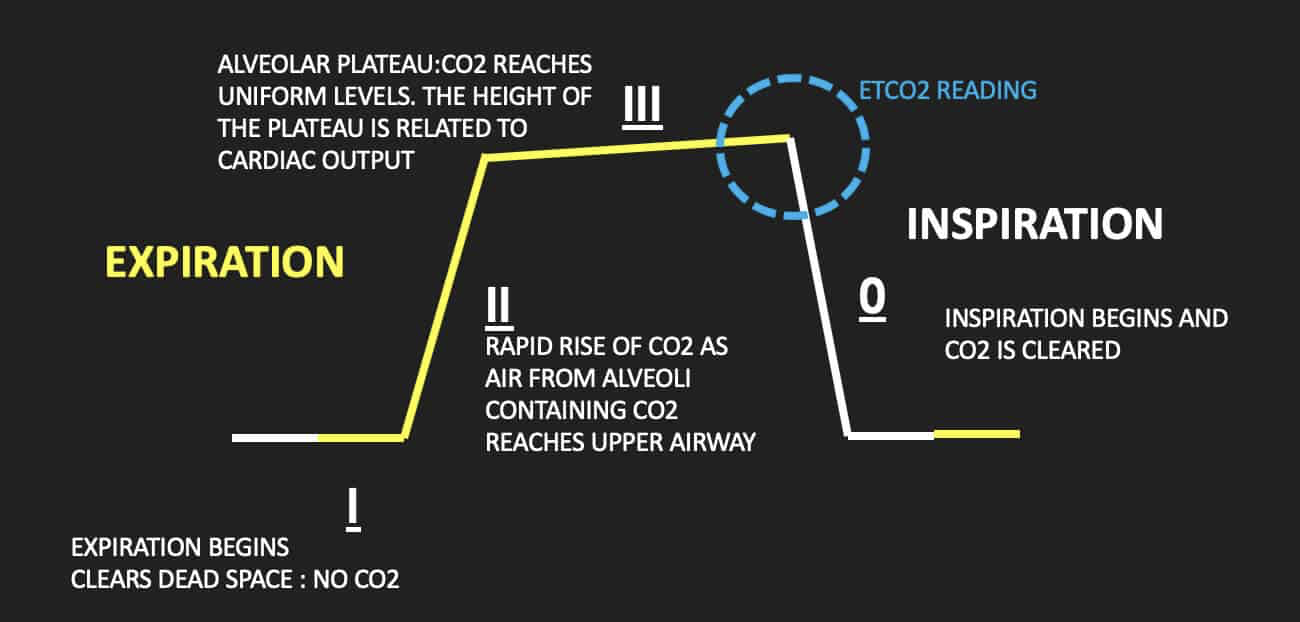
- Angles
- The α angle represents the angle formed between Phase 2 and Phase 3; normally 110 degrees
- Variations in this angle is linked to variations in time constants within the different alveolar units and thus overall V/Q status
- Other factors that affect this angle: cardiac output, airway resistance, and changes in FRC
- The α angle represents the angle formed between Phase 2 and Phase 3; normally 110 degrees
- Clinical Utility of Capnography
- Confirmation of endotracheal tube placement
- Continuous monitoring (loss of exhaled CO₂ = displaced ETT)
- Perfusion during CPR -- effectiveness of resuscitation, ROSC
- Detection of hypoventilation, bradypnea, apnea, and reverse I:E ventilation (shorter time during exhalation)
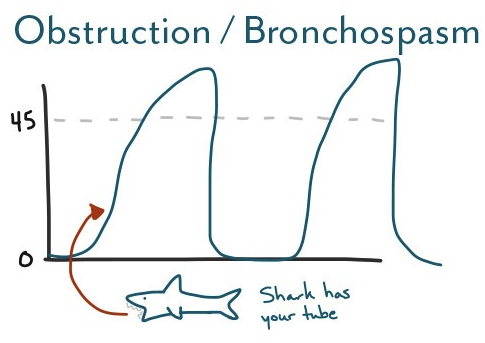
- In Asthma/Chronic Obstructive Pulmonary Disease → uneven alveolar emptying and V/Q mismatch → "Shark-Fin" contour representing airflow obstruction
- Gap between arterial and end-tidal CO₂ is usually negligible in healthy nonintubated patients (usually around 2 to 5 mmHg) - P(a-ET)CO₂
- Cardiac and respiratory pathologies can increase this gap and this can be used to estimate alveolar dead space ventilation
- In conditions such as acute pulmonary embolism, a precipitous drop of end-tidal CO₂ will happen and if the PaCO₂ remains constant, this leads to a significant increase in P(a-ET)CO₂
- Normalization of this gap has been shown as a positive prognostic sign when seen after re-perfusion from tPA
- Other causes of increased P(a-ET)CO₂
- Hypovolemia
- Hemorrhage
- Excessive PEEP
- Early ARDS -- independent risk factor for death
- Negative P(a-ET)CO₂
- Uncommon → verify the validity of the values from capnopgraph and ABG
- Etiologies:
- low frequency and high tidal volume ventilation
- post CABG
- post exercise
- pregnant
- pediatric patients