Physiology of Gas Exchange
Overview of Hypoxemia
- Impairment of perfusion and the matching of ventilation and perfusion results in Hypoxemia
-
Principle mechanisms of hypoxemic respiratory failure can be separated into intrapulmonary and extrapulmonary factors
| Mechanisms | PaO2 | PaCO2 | A-a on RA | A-a on 100% | Intrapulmonary vs Extrapulmonary |
| --------------------------------------------------------------- | ------ | -------------------- | --------- | ----------- | -------------------------------- |
| Low Cardiac Output → Low O₂ delivery | ↓ | ↑ | N | N | Intrapulmonary |
| High Altitude | ↓ | ↓ | N | N | Intrapulmonary |
| Alveolar Hypoventilation | ↓ | ↑ | N | N | Extrapulmonary |
| VQ Mismatch | ↓ | ↓, N, or ↑ | ↑ | Corrects | Extrapulmonary |
| Diffusion Block | ↓ | N or ↓ | ↑ | Corrects | Extrapulmonary |
| Right-to-Left Shunt | ↓ | N or ↓ | ↑ | ↑ | Extrapulmonary | -
Extrapulmonary Factors
- High Altitude
- Low partial pressure of inspired oxygen (PIO₂) which reduces oxygen content (e.g. high altitude -- above 8000 feet) → results in hyperventilation → lower PaCO₂
- A-a gradient is normal and therefore the lung function is normal
- \(P_{AO_{2}} - P_{aO_{2}} = F_{IO_{2}}(P_{atm}-P_{H_{2}O})-P_{aCO_{2}}/R - P_{aO_{2}}\)
- R = the respiratory exchange ratio \((\dot{V}_{O_{2}}/\dot{V}_{CO_{2}})\)
- \(\dot{V}_{O_{2}}\) = Oxygen consumption
- \(\dot{V}_{CO_{2}}\) = Carbon dioxide production
- Decrease in \(F_{IO_{2}}\) or \(P_{atm}\) via travel to altitude will functionally decrease \(P_{AO_{2}}\) and lead to hypoxemia despite normal lung function
- Low Cardiac Output
- Low oxygen delivery to the tissues as a result of low cardiac output resulting in tissue hypoxia → generation of lactic acid (supply/demand mismatch)
- normal oxygen content
- due to the tissues wanting more oxygen, it will be extracted by the tissues more and the amount of deoxygenated blood returning to the lung is higher
- If normal lungs then this is rapidly re-oxygenated
- If impairment in lung oxygenation, blood leaving the lungs may not be fully oxygenated
- DO₂ Cardiac Output x Carrying Capacity
- = Cardiac Output x {(Hb x %saturation of Hb x 1.34 PaO₂ x 0.003
- Carrying capacity is equivalent to oxygen content
- Low oxygen delivery to the tissues as a result of low cardiac output resulting in tissue hypoxia → generation of lactic acid (supply/demand mismatch)
- High Altitude
- Intrapulmonary Factors
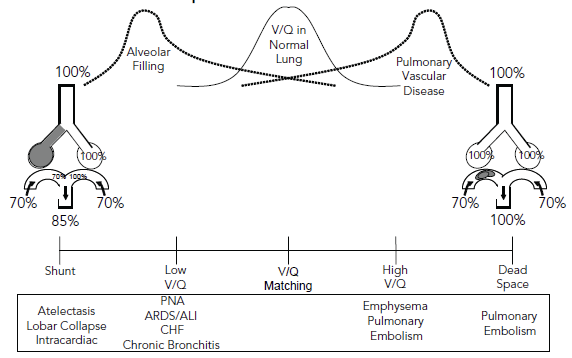
- Shunt
- Perfusion without accompanying ventilation -- can be structural or physiological
- Structural Shunt
- Intracardiac
- right-to-left communication -- PFO, PDA, ASD, VSD
- Intrapulmonary
- abnormal connection between pulmonary arteries and pulmonary veins -- AVM
- Differentiate between intracardiac and intrapulmonary shunts
- Contrast echo w/ air bubbles injected into the venous circulation and visualized in the left atrium
- Timing differentiates between intracardiac and intrapulumonary
- Intracardiac -- within 1 to 3 cardiac cycles
- Intrapulmonary -- within 6 to 8 cardiac cycles - Physiologic Shunt
- Found in states of dense alveolar filling or collapse
- atelectasis or compresive atelectasis (due to abdomen or pleural effusion)
- Pneumothorax
- Central airway obstruction
- In these conditions, hypoxic vasoconstriction reduces much of the blood flow through the nonaerated lung zones but not completely leaving areas of perfusion without ventilation
- Found in states of dense alveolar filling or collapse
- V/Q Mismatch
- Spectrum of diseases
- Most common cause of Hypoxemic Respiratory Failure
- Optimal gas exchange is based on maximally matching ventilation and perfusion that is, a V/Q ratio equal to 1
- In a healthy patient, V/Q ratio is not uniform in the lung but the summation of the 300 million alveoli in a normal distribution around a V/Q ratio equal to 1
- In disease states, regional mismatching of ventilation and perfusion leads to ineffective gas exchange
- Regional vascular dropout
- Emphysema or large pulmonary embolism → high V/Q (nearing dead space physiology) → hypercapnia
- Patchy alveolar filling → low V/Q state (nearing shunt physiology)
- Regional vascular dropout
- Common conditions associated with abnormal V/Q matching
- Pneumonia
- Alveoli fill with purulent material over time → disrupt basement membrane and cellular tight junctions → disruption in alveolar ventilation → low V/Q → hypoxia
- Cardiogenic pulmonary edema and congestive heart failure
- Fluid accumulation in the interstitium and alveolus due to disruption in the direction and rate of fluid exchange due to left heart issues
- Left heart issues → elevated left atrial pressure → capillary hydrostatic changes → fluid accumulation in the interstitium
- Hypoxemia in CHF = multifactorial
- Early on the interstitial fluid causes a diffusion abnormality & low V/Q
- Diffusion abnormality
- interstitial fluid → diffusion abnormality → hypoxemia
- Low V/Q
- interstitial fluid → decrease in lung compliance → regional decline in ventilation → Low V/Q
- interstitial fluid → narrowing of the airways surrounding this region → decline in ventilation → Low V/Q (classic cardiac wheeze on physical examination)
- Diffusion abnormality
- Later → alveolar flooding → low V/Q areas convert to shunt physiology → progressive hypoxemia
- Early on the interstitial fluid causes a diffusion abnormality & low V/Q
- Noncardiogenic pulmonary edema and Acute Respiratory Distress Syndrome
- Fluid accumulation in the interstitium and alveolus due to disruption in the direction and rate of fluid exchange due to changes in oncotic pressure and/or capillary permeability
- Oncotic pressure changes and/or capillary permeability changes → leak of protein and fluid accumulation in the interstitium
- Appearance of classic hyaline membranes lining the alveoli
- Hypoxemia in ARDS = multifactorial
- Early → increased permeability & fluid extravasation → low V/Q
- Later → atelectatic lungs from low ventilation in dependent lungs & overdistention in anterior portions of lungs
- Chest wall restrictions of posterior ribs → decreased compliance
- Pooling of fluid and exudate in posterior lungs → decreased ventilation
- Pneumonia
- Spectrum of diseases
- Diffusion block
- Pulmonary Hypertension
- Interstitial Diseases
- These patients only become hypoxic when they exert themselves as this decreases the time the red blood cell spends in the capillary → decreased time for diffusion to occur
- normally, exertion causes an increase in cardiac output and recruitment of pulmonary vascular units → decreasing pulmonary vascular resistance
- These patients are unable to recruit pulmonary vascular units therefore the flow rates through the capillary bed increase, leading to a decrease in time for uptake of oxygen in the capillary unit
- Alveolar Hypoventilation
- Final common pathway for all causes of respiratory distress
- Alveolar filling processes caused by pneumonia, ARDS, alveolar hemorrhage, CHF usually affect the lung in a heterogenous fashion therefore have both shunt and V/Q mismatch contributing to the hypoxemia
- Shunt