Pneumonia due to Gram-Positive Bacteria
Pneumococcus
Staphylococcus aureus (MRSA & Community-Associated MRSA)
Other Gram-Positive Bacteria
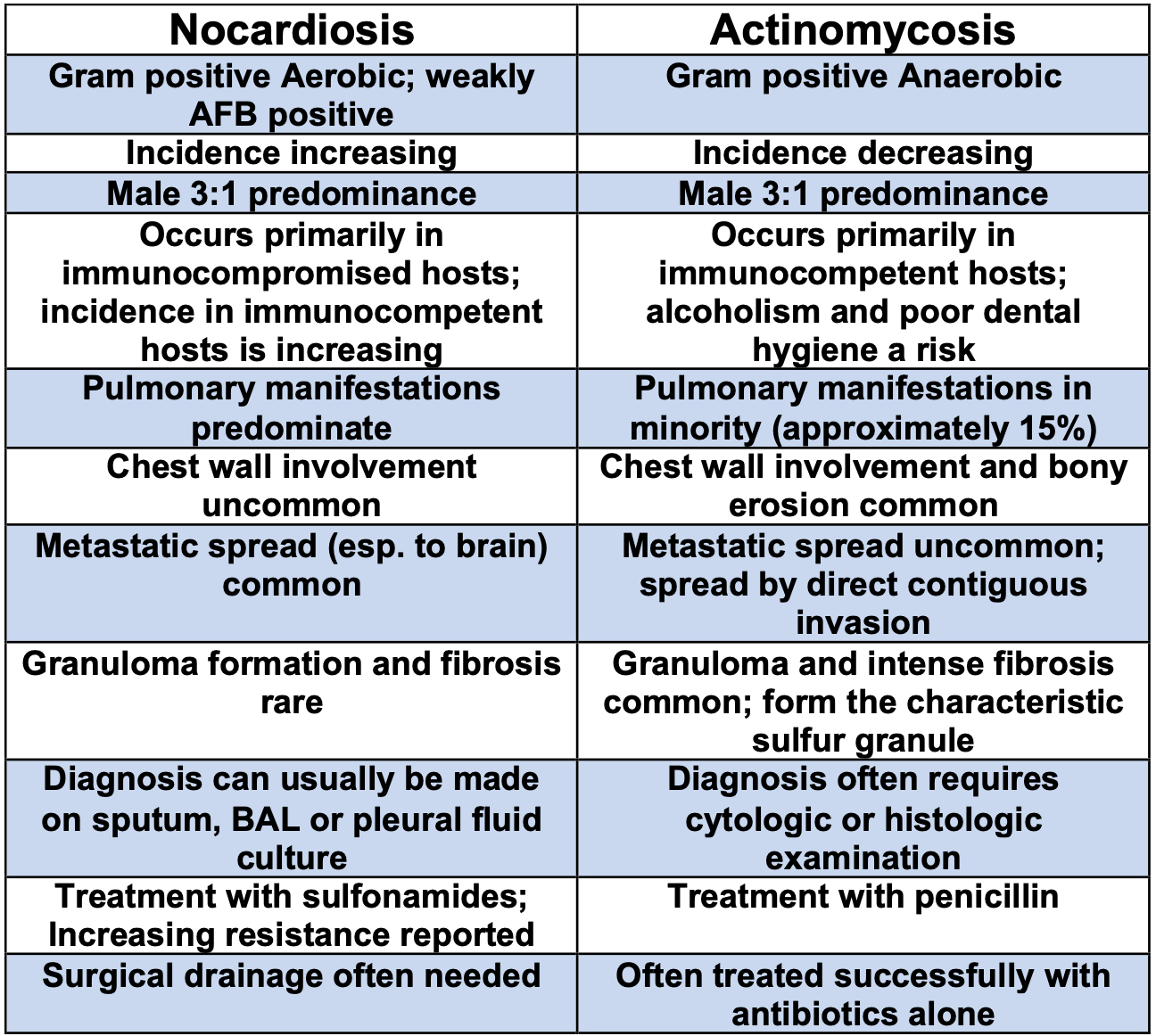
Nocardiosis
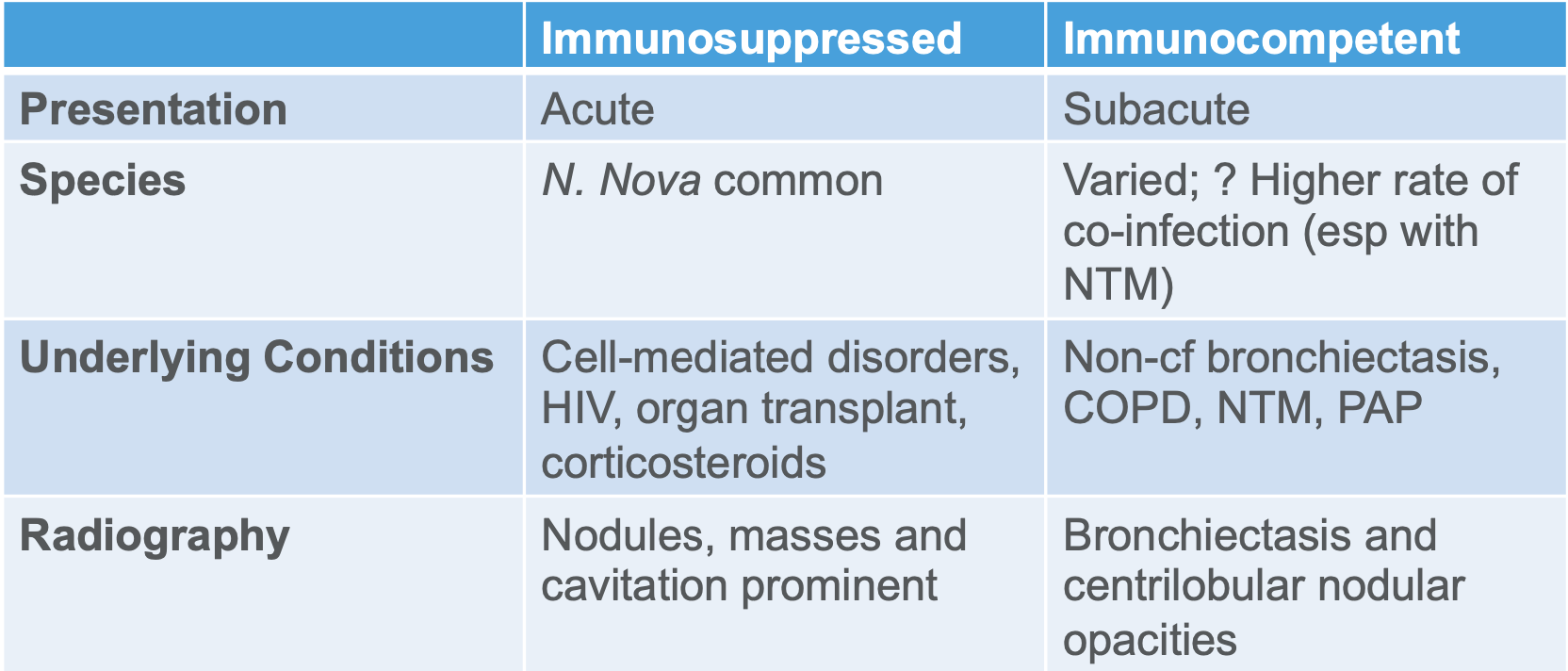
General
-
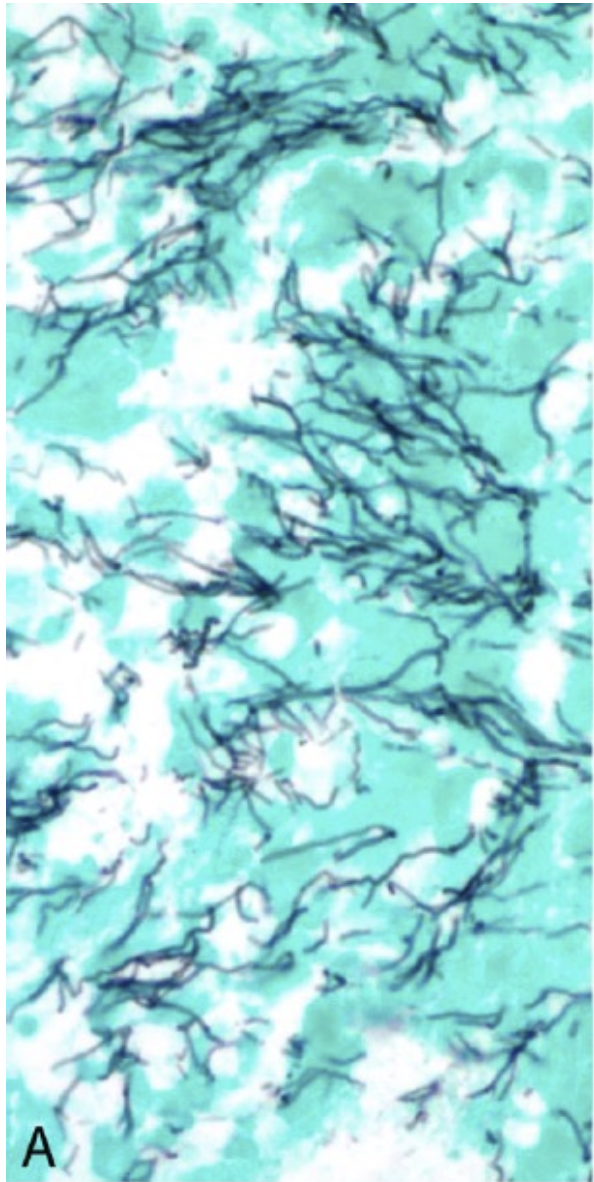
Agent
- Nocardia -- thin, delicate, gram positive aerobic actinomycete bacteria with beaded branching filaments that gives it a hyphae like appearance
- right angle branches
- Seven species a/w human disease
- N. nova, N. asteroids (Type VI) most common
- N. brasileinsis most commonly a/w mycetoma
- Not normal colonizers in the lung
- Very fastidious; weakly acid fast; negative PAS stain
- Romanowsky stain preferred
eosinophilic matrix → pink staining
- Nocardia -- thin, delicate, gram positive aerobic actinomycete bacteria with beaded branching filaments that gives it a hyphae like appearance
-
Transmission
Inhalation in the lungs or less commonly directly into the skin after trauma
Other modes: ingestion or innoculation- Dissemination occurs in approximately 50% of cases of pulmonary nocardiosis at the time of diagnosis
- Risk factors
- Historically opportunistic disease
- 2/3 in immunocompromised patients -- impaired cell-mediated immunity such as HIV (CD4 <100), transplant recipients (especially lung transplant), malignancy (Lymphoma), or those on high-dose chronic steroids, Anti-TNF therapy (monoclonal > soluble)
- immunocompetent patients with underlying pulmonary disease (advanced COPD, bronchiectasis, PAP, granulomatous diseases)
Clinical Manifestations
- Can mimic blastomycosis (lung and skin lesions) or TB (upper-lobe cavitary lesions and weakly positive AFB)
- Most common is subacute pneumonia
- Clinical manifestations of pulmonary nocardiosis are variable and are related to whether the infection produces pneumonia, lung abscess, or cavity, and whether there is pleural involvement
- Other pulmonary manifestations may include pleural effusion, tracheitis, bronchitis, pleuropulmonary fistula, mediastinitis, pericarditis and sinusitis
- Chest x-ray -- dense mass like lingular infiltrate
- High tropism for CNS -- headaches, fever, FND, seizures -> early imaging is paramount -> brain abscess
- Often systemic with more than 2 sites involved -- i.e. extrapulmonary dissemination common
- 50% of pulmonary nocardiosis disseminate to CNS
- All immunocompromised patients with nocardia infection should have a brain CT or MRI as should those with immunocompetence and anything other than cutaneous disease
- 40% have silent dissemination
- Severe nocardiosis -- pulmonary disease with dissemination including the CNS
- Other locations -- skin, bone, muscle
- More common in patients with HIV and alcoholism
- Radiographic Manifestations
- Airspace consolidation common
- Most common feature is cavitation
- Nodules seen more with Nocardia
Diagnosis
- Due to the nodules, masses and cavitation it is often confused with malignancy, rhodococcus equi, aspergillus
- Can often culture; may need bronchoscopy to get good specimens
- culture need to be incubated aerobically for up to 4 weeks
- If smear is positive + immunocompromised patient => disease
- Can get PCR to speed up the diagnosis
Management
-
IV empiric antibiotics -- 2 or 3 agents
TMP/Sulfa- Amikacin
- Linezolid
- Imipenem
- Ertapenem
- Mild to Moderate pulmonary nocardiosis -- TMP-SMX
- resistance more common in patients with underlying lung disease
- Severe pulmonary nocardiosis and/or CNS involvement -- IV TMP-SMX + Amikacin or with the addition of imipenem for CNS disease
- Immunocompromised + moderate to severe pulmonary nocardiosis without CNS -> IV TMP-SMX + Amikacin OR imipenem + Amikacin
- Switch to high-dose oral after 3 to 6 weeks of IV therapy depending on response and sensitivity results
- Because therapy may need to be extended (6 to 12 months or more), resistance is common, and recurrence is frequent despite drugs appropriately selected based on sensitivity patterns, obtaining infectious disease consultation to assist in patient management is encouraged
- Do 2 drugs up front until susceptibility is known especially if its severe disease
- If sulfa allergy -> desensitization or minocycline
Mortality Risk Factors
- Independent risk factors
- Age > 68
- Pulmonary aspergillosis
- Resistance to TMP/SMX
Actinomycosis
General
- Agent
- Actinomyces israelii -- gram positive filamentous anaerobic bacterium
- Acute angles
- easily seen on Pap smear
- Thinner than fungal infections (like aspergillus)
- Reservoir
- normally colonizes in the mouth → aspiration → pneumonia
- other locations: colon, vagina
- Therefore extension of disease from abdominal cavity or neck can occur
- normally colonizes in the mouth → aspiration → pneumonia
- Transmission
- Risk Factors
- Most infections occur in normal hosts
- M > F 3:1
Clinical Manifestations
- Given that the reservoir is in the mouth can be seen initially with an infection of the cervicofacial region that invades into the mediastinum
- Cervicofacial actinomycosis
- Risk factors -- dental caries, gingivitis, DM, immunosuppression, malnutrition, bisphosphonate use and local tissue damage caused by tumor or radiation therapy
- Cervicofacial collections may manifest overlying bluish or reddish discoloration and cutaneous fistulization may occur, with drainage of thick yellow exudate with characteristic sulfur granules
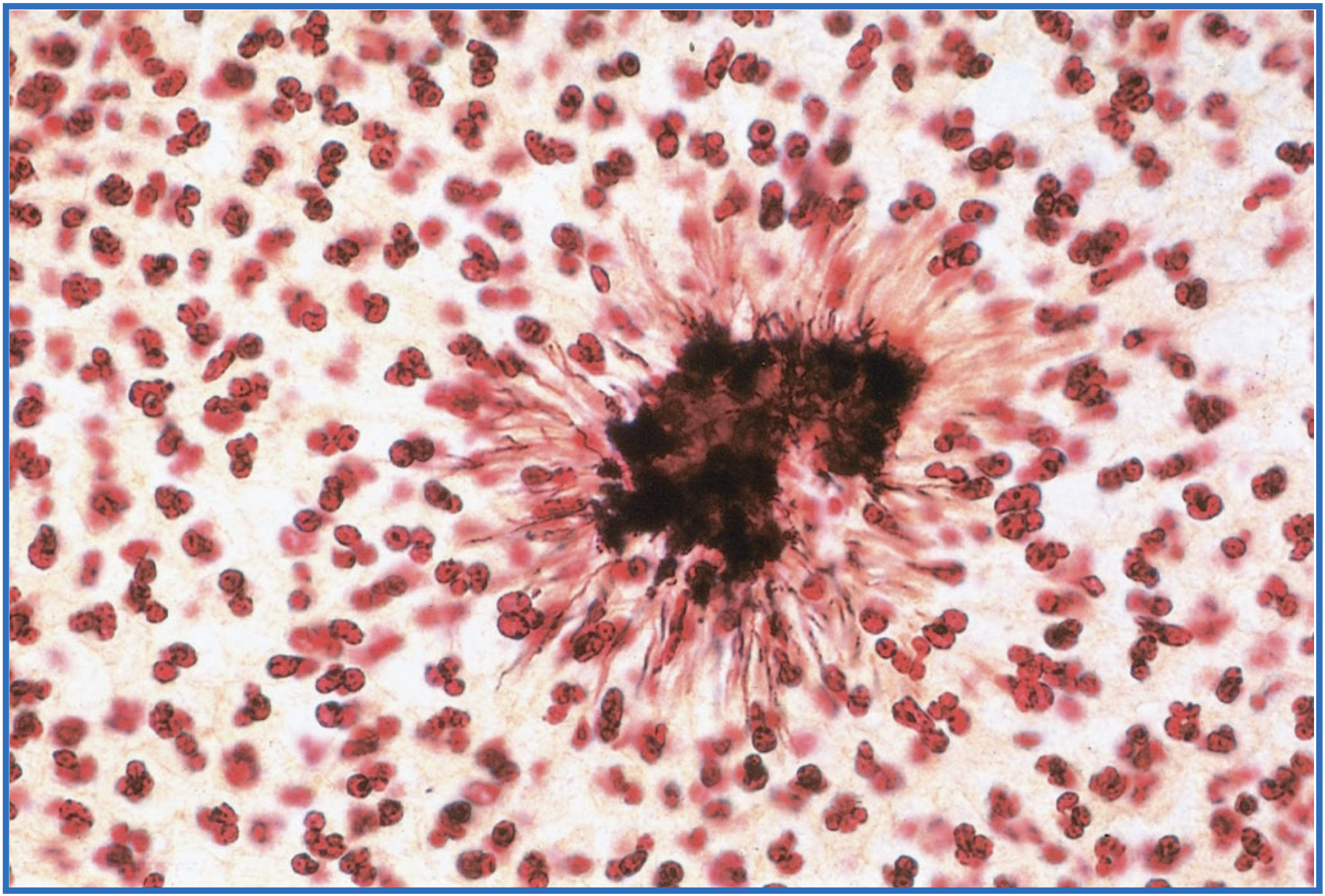
- Sulfur granule surrounded by the proteinaceous material
- Cervicofacial actinomycosis
- Bronchocutaneous fistula highly suggestive
- Often confused with lung cancer and TB
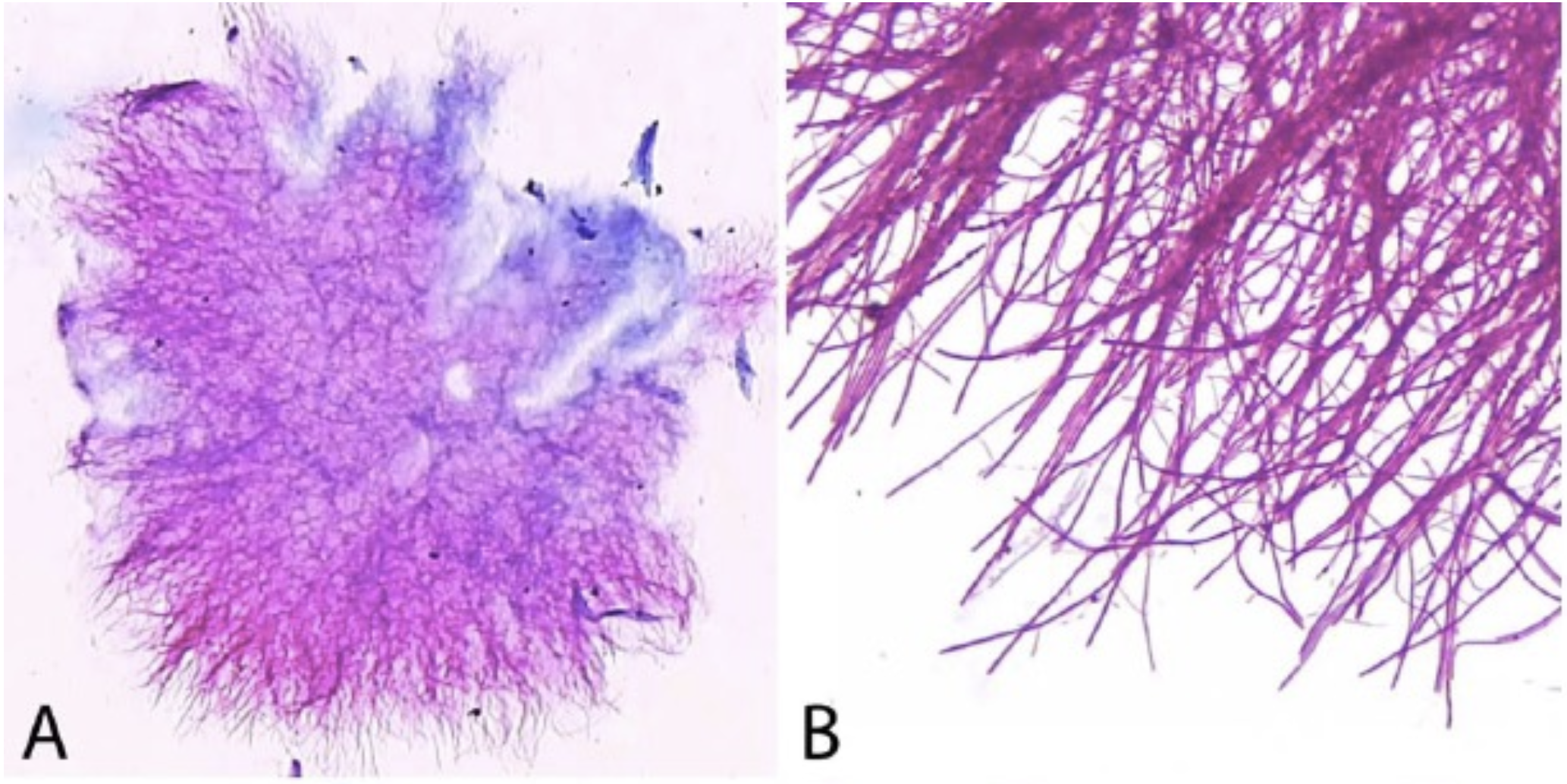
- Microscopy
- AFB negative
- PAS negative
- Radiographic Manifestations
- CT shows patchy airspace consolidation a/w pleural effusion and lymphadenopathy
- Multiple fistulae
- Lung abscess → empyema → osteomyelitis of ribs → chest wall sinus tract formation
- Pleural disease + adenopathy
- Tend to be in periphery and lower lung fields
- Most common feature is cavitation
- Histology
- Sulfur granules
- hard, yellow concretions that are aggregates of mycelial fragments and visible to the naked eye or with low-power microscopy
- Sulfur granules
Management
- Untreated = fatal
- Prolonged therapy needed
- Penicillins
- Usually Zosyn
- If allergic to penicillins -> tetracyclines, clindamycin or erythromycin
- Agents with penicillinase-resistant semisynthetic penicillins such as oxacillin, fluoroquinolones, metronidazole, aminoglycosides, aztreonam, and sulfonamides are poor against Actinomyces